Radiation is a mainstay in the treatment of prostate cancer. In men with localized prostate cancer (confined to the prostate gland), using radiation can help cure the cancer. In men with advanced disease, radiation can improve survival and help to manage pain.
Radiation can be delivered a variety of different ways. For example, there are external beams that can be used to deliver radiation from an external machine into the prostate, radioactive “seeds” that can be implanted, or ways to inject special radioactive isotopes directly into the bloodstream.
In the United States (U.S.), there are older FDA-approved treatments utilizing radioactive isotopes for men with prostate cancer that has spread to the bones to decrease pain, called samarium-153 (brand name Quadramet) and strontium-89 (Metastron). More recently, a bone-targeted alpha particle called radium-223 (brand name Xofigo®) was approved because it leads to longer overall survival in men with symptomatic metastatic castration-resistant bone metastases. These bone-targeted radioisotopes have been useful because prostate cancer commonly spreads to bone. However, those drugs cannot treat other sites of tumors such as in the prostate, lymph nodes, or lung.
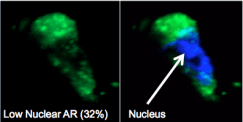
We are also able to use parts of the immune system as a way to deliver radioactive particles or other targeted cancer treatments to the prostate cancer. We have engineered very specific monoclonal antibodies and molecules that will bind only to PSMA, leading to the opportunity for “molecularly targeted” radiotherapy for prostate cancer. When we combine immunotherapy with monoclonal antibodies with radioactive isotopes, we call the treatment approach radioimmunotherapy. Radioimmunotherapy involves attaching a radioactive isotope (such as Lutetium 177) to a cancer-targeting antibody or small molecule that binds only to a specific cancer-related molecule on a tumor cell. This is similar to a “lock and key” scenario, where the antibody or molecule serves as a key that will only recognize a very specific lock (the cancer-related molecule). In prostate cancer, nearly all cells have a specific “lock” that lives on the surface of each cell called prostate-specific membrane antigen (PSMA).
 For nearly 15 years, we have been utilizing a monoclonal antibody known as J591, which is a version of a specific key that will only recognize and enter cells with the specific lock PSMA. We successfully utilized this antibody tagged with small radioactive particles to either visualize or treat prostate cancer tumors within the prostate, bone, lymph nodes, and other sites in the body. Our initial studies demonstrated safety and signaled anti-tumor efficacy. In addition, we showed that the antibody went to virtually all sites of tumors (sometimes discovering new ones) and did not target other normal organs (with the exception of the liver which helps clear the drug from the body). Subsequently, our larger studies have shown responses in larger numbers of patients. In Europe, physicians picked up on our results and Lutetium 177 (also known as Lu-177, 177-Lu or 177 Lutetium) has become a very popular radioactive particle that can be directed to prostate cancer via PSMA. It has been used to kill prostate cancer cells and treat hundreds of prostate cancer patients. This commonly-used approach uses a small molecule which recognizes PSMA to deliver Lu-177 to prostate cancer cells (termed radioligand therapy or radioimmunotherapy therapy).
For nearly 15 years, we have been utilizing a monoclonal antibody known as J591, which is a version of a specific key that will only recognize and enter cells with the specific lock PSMA. We successfully utilized this antibody tagged with small radioactive particles to either visualize or treat prostate cancer tumors within the prostate, bone, lymph nodes, and other sites in the body. Our initial studies demonstrated safety and signaled anti-tumor efficacy. In addition, we showed that the antibody went to virtually all sites of tumors (sometimes discovering new ones) and did not target other normal organs (with the exception of the liver which helps clear the drug from the body). Subsequently, our larger studies have shown responses in larger numbers of patients. In Europe, physicians picked up on our results and Lutetium 177 (also known as Lu-177, 177-Lu or 177 Lutetium) has become a very popular radioactive particle that can be directed to prostate cancer via PSMA. It has been used to kill prostate cancer cells and treat hundreds of prostate cancer patients. This commonly-used approach uses a small molecule which recognizes PSMA to deliver Lu-177 to prostate cancer cells (termed radioligand therapy or radioimmunotherapy therapy).
Lutetium-177 PSMA therapy is associated with a good prostate cancer response and many men travel from all over the world to Europe in order to access this treatment. In the U.S. it is only available via clinical trials, and for more than 10 years, Weill Cornell Medicine and NewYork-Presbyterian have been one of the few centers in the U.S. to offer Lutetium 177 and other targeted treatments using radioactive particles.
Learn more about how this treatment works in this video:
 Dr. Scott Tagawa presented
Dr. Scott Tagawa presented 
 The bladder is an organ comprised of several layers of cells, and its main job is to store urine. When it’s full, it lets you know. But, chances are there are many other things about the bladder that you may not know. In honor of bladder cancer awareness month in May, here are 9 facts:
The bladder is an organ comprised of several layers of cells, and its main job is to store urine. When it’s full, it lets you know. But, chances are there are many other things about the bladder that you may not know. In honor of bladder cancer awareness month in May, here are 9 facts: