 Babak B. Navi, MD, MS
Babak B. Navi, MD, MS
Stroke Center Director
Assistant Professor of Neurology
Weill Cornell Medicine | NewYork-Presbyterian
Over the past decade, there has been tremendous progress in cancer therapeutics. This includes targeted agents that act on specific receptors in cancer cells, immunotherapy which harnesses the body’s immune system to attack cancer cells, and personalized medicine whereby oncologists use different combinations of cancer drugs to optimize the chance of success based on the molecular profile of the tumor. These amazing scientific advances have led to prolonged survival for people with several cancer types, and it is possible that in the not-too-distant future, cancer will become more of a chronic disease with periodic flare-ups similar to what has occurred with diabetes and HIV. However, with this paradigm shift, long-term quality of life and well-being has become more important, and preventing diseases and complications that can affect these factors is paramount.
Stroke is the leading cause of disability in the United States. In addition, in many parts of the world, including Asia, it is the leading cause of death. In the United States alone, 800,000 people each year suffer stroke and this number is expected to rise as average life expectancy increases. Many factors can increase a person’s risk for stroke including age, hypertension, diabetes, high cholesterol, obesity, and smoking. Besides these traditional stroke risk factors, we now know that cancer and its treatments also increase the risk of stroke. In particular, patients with certain types of cancer, such as lung, pancreatic, and bladder cancers, as well as patients with metastatic disease, tend to have the highest risk. For instance, elderly patients with newly-diagnosed lung cancer face roughly an 8% risk of stroke in the first year after being diagnosed with cancer. In addition, cancer patients’ stroke risk varies with time and is highest in the first 3 months after diagnosis, when some cancer patients face up to a 3-fold higher risk of stroke than usual. It also turns out that certain necessary and potentially life-saving cancer treatments, including some forms of chemotherapy and radiation, can increase stroke risk.
At the moment, the exact reasons why cancer patients face a heightened risk of stroke are unclear. It is well known that circulating cancer cells can alter individuals’ clotting systems to promote clot formation but exactly how they do this is uncertain. Furthermore, doctors know that certain chemotherapy and radiotherapy treatments can damage blood vessels, but once again, the exact mechanisms underlying these processes are poorly understood.
At Weill Cornell Medicine and NewYork-Presbyterian, my team is actively working to determine what the exact risks of stroke are in people with newly diagnosed cancer, what clinical factors and biomarkers in blood can help doctors identify high-risk patients, and what the optimal strategies are to prevent and treat stroke in cancer patients. One particular study that we are currently enrolling into is entitled MOST-Cancer. This study uses cutting-edge ultrasound and blood tests to evaluate the predictors and mechanisms of stroke in people with cancer. If you or a loved one has cancer and are interested in learning more about these studies, please email our team at stroketrials@med.cornell.edu or call 212-746-6757.
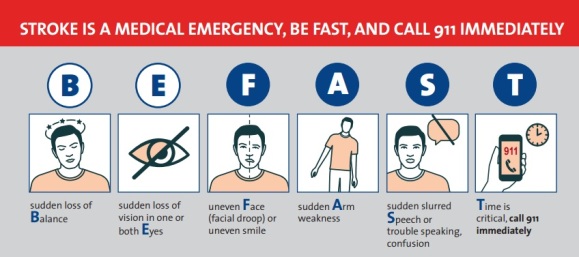
May is National Stroke Awareness Month. The main intent of this campaign is to raise awareness about the symptoms and signs of stroke and to educate the public to call 911 if they suspect stroke. The most popular campaign is FAST, which stands for Face, Arm, Speech, and Time – Time to call 911.
If you or a companion develops unexplained facial asymmetry, arm weakness, or speech changes, you should call 911 immediately so that an ambulance is activated to provide rapid delivery to the closest stroke center. This is imperative as there are medicines and surgical procedures that have been proven to improve outcomes after stroke but these are only effective in the first few hours after stroke onset. Therefore, if stroke is suspected, do not hesitate, call 911, as it could be life saving!
Furthermore, I recommend that cancer patients have a frank discussion with their doctors about their individual risks for stroke and other cardiovascular diseases, as well as potential strategies to reduce their risks through medicines and lifestyle modifications.
We’ve made great strides in oncological care so that patients routinely get cured or live many years with their disease. Therefore, it is now time that we turn our attention to long-term quality of life, and in particular, to preventing stroke and the other secondary complications of cancer.


 We grow up learning certain truths regarding the need to brush our teeth at least twice a day and visit the dentist on a regular basis, but during cancer treatment, our mouth needs can change.
We grow up learning certain truths regarding the need to brush our teeth at least twice a day and visit the dentist on a regular basis, but during cancer treatment, our mouth needs can change.