Last week, approximately 100 of the leading experts in genitourinary (GU) cancer research and treatment converged in Prague in the Czech Republic for the 114th Annual American Urology Association (AUA) Meeting. The AUA’s mission is “to promote the highest standards of urological clinical care through education, research and in the formulation of health care policy.”
Last week, approximately 100 of the leading experts in genitourinary (GU) cancer research and treatment converged in Prague in the Czech Republic for the 114th Annual American Urology Association (AUA) Meeting. The AUA’s mission is “to promote the highest standards of urological clinical care through education, research and in the formulation of health care policy.”
The AUA has over 22,000 members from across the country, and many of the Weill Cornell Medicine/NewYork-Presbyterian GU physicians serve as members of the New York chapter. At this year’s meeting, doctors David Nanus, Jim Hu, and Scott Tagawa were invited to present on the latest standards in screening and treatment for prostate, bladder and kidney cancers.
 On Thursday, September 15th, Dr. Jim Hu spoke about the screening controversy surrounding the early detection of prostate cancer and how this influences present day practice and the medical care men are receiving. We have a number of different screening tools available to detect prostate cancer and distinguish between aggressive and non-aggressive sub-types. One of the most common and least invasive ways to screen for prostate cancer is through Prostate Specific Antigen (PSA) testing, but this is controversial because some argue that it leads to false positives, or the detection of cancers that are very slow growing and may never need treatment. Most physicians and scientists agree that PSA testing isn’t perfect, but research shows that it can be a very good screening indicator when used in conjunction with physical exams, biomarkers and imaging tools. In addition, analysis of a recent study demonstrated that surveillance remains an option for some men with little difference in 10-year survival in those that choose treatment with either surgery or radiation, though there are tradeoffs in terms of a higher likelihood of developing advanced cancer in those that avoid more aggressive treatment.
On Thursday, September 15th, Dr. Jim Hu spoke about the screening controversy surrounding the early detection of prostate cancer and how this influences present day practice and the medical care men are receiving. We have a number of different screening tools available to detect prostate cancer and distinguish between aggressive and non-aggressive sub-types. One of the most common and least invasive ways to screen for prostate cancer is through Prostate Specific Antigen (PSA) testing, but this is controversial because some argue that it leads to false positives, or the detection of cancers that are very slow growing and may never need treatment. Most physicians and scientists agree that PSA testing isn’t perfect, but research shows that it can be a very good screening indicator when used in conjunction with physical exams, biomarkers and imaging tools. In addition, analysis of a recent study demonstrated that surveillance remains an option for some men with little difference in 10-year survival in those that choose treatment with either surgery or radiation, though there are tradeoffs in terms of a higher likelihood of developing advanced cancer in those that avoid more aggressive treatment.
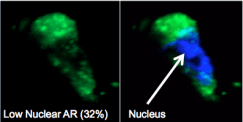
Later that day, Dr. Scott Tagawa provided an update on the impact of chemotherapy in treating prostate cancer – a modality that was once thought to be a treatment last-resort. Chemo is now a standard much earlier on during cancer care and people are living longer, and feeling better as a result. In particular, the earlier use of a short course of chemotherapy at the time that men initially present to the clinic with advance prostate cancer leads to a significant increase in survival combined with better overall quality of life in the longer-term. The two taxane chemotherapy drugs proven to be successful in prostate cancer are docetaxel and cabazitaxel, and the latest research on these drugs seeks to answer questions regarding for whom and when these treatments will be benefit. At Weill Cornell/NYP we are leading the field in this research and developing hi-tech biomarkers to determine sensitivity and resistance.
Dr. David Nanus presented on Friday and highlighted the latest advances in treating urothelial cancers of the kidney and bladder. After nearly three decades with no new FDA drug approvals for bladder cancer, in 2016 we witnessed great treatment advances for bladder cancer. With immunotherapy, chemotherapy and genomics, we’re now on the cusp of precision medicine. The combination of these approaches with novel treatments is improving the lives of many of our patients with advanced urothelial carcinoma. We are now able to offer complete tumor and germline (inherited) genomic analysis as part of research studies that in the near term will translate to selecting the optimal treatment strategy for each individual patient.




 Dr. Scott Tagawa presented
Dr. Scott Tagawa presented